Clinician's Guide to Medical Aid in Dying
Under Vermont's Act 39
Author: Jaina Clough, M.D.
Contributors: Diana Barnard, M.D. Toni Kaeding, MS RN, Betsy Walkerman, Esq
This Guide is intended as a practical tool for clinicians as they support patients who are considering
or actively pursuing medical aid in dying (MAID).
Contributors: Diana Barnard, M.D. Toni Kaeding, MS RN, Betsy Walkerman, Esq
This Guide is intended as a practical tool for clinicians as they support patients who are considering
or actively pursuing medical aid in dying (MAID).
What is Medical Aid in Dying? Medical Aid in Dying (MAID) gives adults who are terminally ill and who are capable of making their own decisions the option to receive prescription medication to bring about a peaceful death at the time of the patient's choosing. The medication must be self-administered. MAID is available under Vermont's Act 39, which was adopted in 2013. MAID is sometimes called "End-of-Life Choice" or "Death with Dignity." MAID is legal in 11 US jurisdictions: California, Colorado, District of Columbia, Hawaii, Maine, New Jersey, New Mexico, Oregon, Vermont, Washington and Montana (legal under court ruling). |
MAID in the Context of End-of-Life CareMedical aid in dying is one component of patient-centered care for those with a terminal illness. All patients with terminal and serious illness should have access to palliative and end-of-life care that includes:
This care can be provided through:
|
The Patient Choices Vermont Helpline is Here for YouFor Doctors: PCV can help you navigate the process of discussing MAID with patients, complete the Act 39 process, and prescribe. PCV staff can connect doctors who have clinical questions to experienced prescribers. For Hospice Personnel: The Helpline can assist with understanding how to guide patients through their process, and with procedural questions. For Patients: Helpline personnel can assist you with how to communicate with your medical team, family and hospice, and can answer questions about Act 39 eligibility and process. The PCV Helpline is staffed by a nurse and a social worker, with access to doctors who have medical aid in dying experience. Medical Aid in Dying Brochures: You may find it helpful to provide this simple brochure to patients. Order your free supply through our Contact Page. Wayfinders Network: PCV's network of Wayfinders may be able to help patients and families navigate the process. Click here for a list. |

|
How to Have Conversations about MAID, Patient Concerns, and Care Options
These conversation may occur with doctors, nurses, social workers or hospice providers.
Understanding Requests for MAID:
- A request for MAID is often an expression of worry or uncertainty about dying.
- If a person is asking about MAID, a clinician should further explore the patient’s understanding of their illness and the future, as well as their reasons for requesting MAID.
- Exploring suffering, or fear of future suffering, is always a priority when caring for patients with serious illness. These conversations allow us to better understand our patients and how best to meet their needs, whether or not the patient ultimately pursues MAID.
Common Patient Concerns:
Survey results from patients in Oregon participating in medical aid in dying, 2019 (188 respondents)
Less able to engage in activities that make life enjoyable |
170 |
90.4% |
Losing autonomy |
163 |
86.7% |
Losing dignity |
136 |
72.3% |
Burden on family, friends, caregivers |
111 |
59.0% |
Losing control of bodily functions |
74 |
39.4% |
Inadequate pain control (or fear of) |
62 |
33.0% |
Financial concerns |
14 |
7.4% |
Questions you can ask to explore a patient's suffering:
- "What does suffering/burden mean to you?”
- “What are you most worried about when you consider the end of your life?”
- “How would you know when the right time might be to hasten your death?”
- “What is an unacceptable quality of life for you?”
Responding to requests for Act 39/MAID (or questions about it):
The most important statement a clinician can say is "Tell me more about that."
Patient might say: |
Clinician might say: |
I've heard about that law. |
Are you thinking about Act 39, medical aid in dying? What is your understanding of the law/Act 39/MAID? |
Can you help me end it when the time comes? |
Can you tell me more about what you are thinking? I will be here to support you through the end of your life, including the care you choose and medical aid in dying if you decide to pursue it. |
I don't want to suffer. I want to end it when the time comes. |
What are you most worried about when you say "suffering." What is most important to you when you consider the end of your life? What has been your experience with serious illness or death and dying? |
Is the Patient Eligible for Act 39/MAID?
Act 39 eligibility requirements:
To qualify for MAID under the legal requirements of Act 39, a patient must:
- Be 18 or older
- Be terminally ill, with a prognosis of six months or less to live
- Make a voluntary request
- Have decision making capacity
- Have a clear understanding of diagnosis, prognosis, treatments for condition, and palliative care options
- Be able to self-administer the prescribed dose of life-ending medication
Change: The physician is no longer required to determine residency.
Legislation passed on May 2, 2023 has eliminated the residency requirement.
The patient must be able to self-administer the medication in order to be eligible. Clinicians should review:
- If taking by mouth, the patient should have the ability to drink and swallow the medication.
- If taking per gastric tube, the patient should have the ability to utilize a syringe to administer the medication through the gastric tube.
- If taking rectally, the patient should have the ability to coordinate use of a syringe to administer the medication through the rectal tube.
Clinical Considerations and Red Flags
Cognitive Impairment
With any serious illness progression, a person may develop cognitive impairment that impacts their decision-making capacity and understanding of consequences. A person may be determined to be eligible, go through the approval process, then become ineligible to proceed with MAID if cognitively impaired.
Inability to self-administer
Inability to self-administer can occur because of disease processes that limit a person’s physical ability to either swallow a medication or hold a syringe to self-administer through a G tube. This can be related either to prognostic factors (ie, a person loses the ability to swallow because they are approaching the final days or weeks of life) or disease factors (such as a neurodegenerative process such as ALS or an esophageal mass that limits ability to swallow).
Efficacy of MAID medication may be limited by gut issues
|
Limiting conditions include:
|
Red flags raise risk of complications
|
If there are red flags that suggest difficulty with ingestion:
|
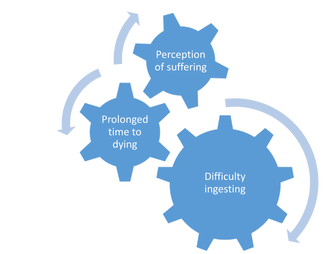
Complications can be inter-related
Difficulty ingesting, or regurgitating, the medication may result in prolonged time to dying.
|
Prescribing Physician - Act 39 Required Procedure
The prescribing physician is responsible for completing a set of specific steps and documenting them in the patient's medical record before a prescription for MAID can be written.
The Vermont Department of Health Forms serve as a convenient checklist. Click on the forms to link and download these pages.
Physicians who are new to the process may want to review the steps, as outlined below:
The Process Starts With
Patient's First Oral Request to the physician
Patient's First Oral Request to the physician
The following steps all have to be taken after first oral request and before prescription can be written, but not necessarily in this order.
Note About Telemedicine: Telemedicine may be used to accomplish any part of the process, as long as the appropriate determinations can be made by this means under normal telemedicine guidelines. For the Act 39 process, telemedicine means with video.
Note About Telemedicine: Telemedicine may be used to accomplish any part of the process, as long as the appropriate determinations can be made by this means under normal telemedicine guidelines. For the Act 39 process, telemedicine means with video.
Physician confirms that the patient meets the Act 39 requirements:
Physician examines the patient and their medical history and determines that the patient is:
- suffering from a terminal disease with a prognosis of six months or less to live,
- capable of making and communicating their decision,
- making an informed decision,
- making a voluntary request for medication to hasten their death, and
- is 18 years or older.
Patient examination:
The prescribing physician must either perform a physical examination of the patient or review the medical record of another physician's physical examination as part of the above requirements.
Patient receives all relevant information:
The physician informs the patient, both verbally and in writing, of all the following:
- the patient's medical diagnosis,
- the patient's prognosis,
- the range of treatment options appropriate for the patient and the patient's diagnosis,
- all feasible end-of-life services, including palliative care, comfort care, hospice care, and pain control,
- the range of possible results, including potential risks associated with taking the medication to be prescribed,
- the probable result of taking the medication to be prescribed, and
- that the patient may rescind the request at any time and in any manner.
Verification regarding capacity:
The physician either verifies that the patient does not have impaired judgment or refers the patient for an evaluation by a psychiatrist, psychologist, or clinical social worker for confirmation that the patient is capable and does not have impaired judgment.
Second physician confirmation:
The patient gets an appointment with the second physician and the second physician confirms:
- the patient’s diagnosis,
- the patient’s prognosis, and
- that the patient is capable, acting voluntarily, and has made an informed decision.
Patient makes a written request with independent confirmation:
The patient makes a written request for the medication witnessed by two independent individuals who affirm that the patient appeared to understand the nature of the document and to be free from duress or undue influence at the time the request was signed. Click here for the Vermont Department of Health Form for the patient's written request.
Patient's Second Oral Request:
Patient makes second oral request to the prescribing physician.
This must be at least 15 days after the first oral request.
Patient makes second oral request to the prescribing physician.
This must be at least 15 days after the first oral request.
Prescribing physician's steps prior to writing prescription:
- Offer the patient the opportunity to rescind the request. Note that the patient has the option to do this at any time and has the option not to use the medication even after filling the prescription.
- Confirm that the patient is making an informed decision.
- Record all of the above, including dates and times of each step and the medication prescribed, in the patient's medical record.
- File the required reports with the Department of Health. These reports include a checklist of all the above steps. Links to these forms are above in the green section where the forms are shown.
- When completing the death certificate for a patient who has utilized MAID, the cause of death is the underlying terminal illness. Medical aid in dying is not documented on the death certificate.
Physician Writes Prescription
It is strongly recommended that physicians contact the pharmacist who fills prescriptions in Vermont ahead of time, as processing can take a few days. It is also recommended to check the current formulation with the pharmacist or a knowledgeable doctor. The PCV Helpline can connect clinicians with Vermont doctors who can provide current prescription information.
Helpline number: 802-448-0542 or [email protected]
It is strongly recommended that physicians contact the pharmacist who fills prescriptions in Vermont ahead of time, as processing can take a few days. It is also recommended to check the current formulation with the pharmacist or a knowledgeable doctor. The PCV Helpline can connect clinicians with Vermont doctors who can provide current prescription information.
Helpline number: 802-448-0542 or [email protected]
Prescribing Physician - Important Next Steps
DNR/COLST Orders Must be in Place
DNR/COLST orders must be in place for all patients planning to use medical aid in dying. This provides clear instructions to any medical person attending the death.
MAID Pharmacology
The current recommended prescription is a compound: Five medications are provided in a powder form (in capsules) to be mixed as a drink. A compounding pharmacy is required to fill the prescription (see below).
The specific recommended formulation may have changed, so even experienced providers are strongly encouraged to check before prescribing.
Prescribers should contact Patient Choices Vermont (PCV) for the current prescription details. 802-448-0542 or [email protected].
The specific recommended formulation may have changed, so even experienced providers are strongly encouraged to check before prescribing.
Prescribers should contact Patient Choices Vermont (PCV) for the current prescription details. 802-448-0542 or [email protected].
Pharmacy Contact Information
|
Hospice is Highly Recommended
It is highly recommended that the patient be enrolled in hospice and that their services be arranged for the day the patient plans to use the medication. This not only provides support for the patient and family, but it ensures that an authorized person will be there to pronounce death.
Without hospice support, the family would need to call their local EMTs for transport of remains to a medical facility where death can be pronounced. In that case, the family should have in their possession a copy of the DNR/COLST and the At 39 paperwork so that the EMTs will have no concerns that the death might be suspicious.
Without hospice support, the family would need to call their local EMTs for transport of remains to a medical facility where death can be pronounced. In that case, the family should have in their possession a copy of the DNR/COLST and the At 39 paperwork so that the EMTs will have no concerns that the death might be suspicious.
Special Procedures - Clinical Considerations
The prescribing doctor should review any relevant clinical considerations and make appropriate arrangements for the planned use of medical aid in dying. These include:
- Pacemakers and defibrillators: The hospice nurse should stop the functioning of these devices before medication is taken.
- Gut Issues: Any special requirements based on the ability of the patient to swallow or absorb the medication.
Instructions for Patients, Families, Hospice
|
We highly recommend that clinicians provide the patient and family with the instructions that can be downloaded by clicking on the box to the right. This is a standard set of instructions development by Dr. Jaina Clough, Dr. Zail Berry and Dr. Diana Barnard in collaboration with PCV and various nursing and hospice volunteers. The pharmacy you use has also been asked to use this standard set of instructions. Note to Doctors: It is your responsibility to confirm that these standard instructions are appropriate for your patient. If your patient has any special condition or circumstances that would dictate a variation of these instructions, it remains your responsibility to provide the appropriate instructions to the patient. |
Patient instructions for day of ingestion
|
Overview of patient instructions on day of self-administration (See right for link to detailed instructions) :
Time to dying: The average time to dying using the current medication protocol is 1.1 hours. The time to dying may vary depending on multiple patient factors (cardiopulmonary physiology, nutritional status, ability to ingest complete dose of medication).
|
Detailed patient instruction PDF
Source: American Clinician's Academy on Medical Aid in Dying Video enactment of day of ingestion
Source: American Clinicians Academy on Medical Aid in Dying |
Educating and supporting patients and families
|
Questions to educate and support patients and families considering MAID:
|
What to expect after ingestion
Family Videos: Patients and their families may find PCV videos to be helpful as they navigate this process. Link to videos. |
Complications and contingency plans
|
Complications
The current medication formula has been developed to deliver the result of a comfortable and peaceful hastening of death. The results are consistently as expected, and complications are rare. Perception of adverse outcomes is often related to expectations. For example, if a patient (and their family) is anticipating an immediate death from utilizing MAID, a 2 hour dying process may be perceived as unexpectedly long. It is important that the physician and patient review possible red flags, as outlined above in order to avoid complications such as incomplete ingestion (thus resulting in sedation with an uncertain timeline of death), or difficulty absorbing the medication. |
Prepare for complications with contingency plans
|
Education and support if a person is unable to proceed with MAID
Prognosis or disease progression may limit a person from proceeding with MAID
- Change in cognition or worsening dysphagia may lead to recommendation to avoid MAID.
- A prognosis longer than six months may surprise a patient who identifies with feeling terminally ill but does not qualify for MAID.
- Inability to proceed with MAID for either reason can be a source of grief, loss and fear for patients.
- Patients and families may have ambivalence about MAID. Provide referrals to social workers or other counselors.
- Anticipate patient and family emotion ( a wide variety is possible: disappointment, relief, grief, fear, loss of control).
- Always return to patient values and offer alternative plans to address suffering and provide support.
Act 39 is Completely Voluntary: The final decision rests with the patient
The patient can decide whether and when to take the medication. Many people are comforted by having the option in hand, but either decide not to use it or their disease simply runs its course.
Clinicians' Responsibilities
Participation in Act 39 is voluntary. However, eligible patients have a right to know about this option
Act 39 is Voluntary: Under Act 39 participation by any clinician is voluntary.
Patient Right to Information:
At the same time, the patient has the right to be informed of all relevant options for care and treatment. This is specified in Vermont's Patient's bill of rights for palliative care and pain management (18V.S.A.Section 1871), which states in relevant part:
(a) A patient has the right to be informed of all evidence-based options for care and treatment, including palliative care, in order to make a fully informed patient choice.
(b) A patient with a terminal illness has the right to be informed by a clinician of all available options related to terminal care; to be able to request any, all, or none of these options; and to expect and receive supportive care for the specific option or options available.
(c) A patient with pain has the right to request or reject the use of any or all treatments in order to relieve his or her pain.
(d) A patient with a chronic condition has the right to competent and compassionate medical assistance in managing his or her physical and emotional symptoms.
This means that it is the doctor's responsibility to make sure that patients who qualify for MAID are aware of its availability and are provided with the level of information enables them to make informed decisions about treatment and care.
When completing the death certificate for a patient who has utilized MAID, the cause of death is the underlying terminal illness. Medical aid in dying is not documented on the death certificate.
Patient Right to Information:
At the same time, the patient has the right to be informed of all relevant options for care and treatment. This is specified in Vermont's Patient's bill of rights for palliative care and pain management (18V.S.A.Section 1871), which states in relevant part:
(a) A patient has the right to be informed of all evidence-based options for care and treatment, including palliative care, in order to make a fully informed patient choice.
(b) A patient with a terminal illness has the right to be informed by a clinician of all available options related to terminal care; to be able to request any, all, or none of these options; and to expect and receive supportive care for the specific option or options available.
(c) A patient with pain has the right to request or reject the use of any or all treatments in order to relieve his or her pain.
(d) A patient with a chronic condition has the right to competent and compassionate medical assistance in managing his or her physical and emotional symptoms.
This means that it is the doctor's responsibility to make sure that patients who qualify for MAID are aware of its availability and are provided with the level of information enables them to make informed decisions about treatment and care.
When completing the death certificate for a patient who has utilized MAID, the cause of death is the underlying terminal illness. Medical aid in dying is not documented on the death certificate.
Suggested clinician approach to patient conversations
- Listen for Patient Concerns: Is the patient expressing worries about their care in the final phases of life, about moving to a nursing home, about having family members care for their personal needs.
- All Options: Let the patient know that they are entitled to know of all their options, including treatment, comfort care, medications, personal assistance, and hospice care.
- Medical Aid in Dying: Discuss the MAID option as one of several in a range of approaches to provide comfort. You might say: "Some people adapt well to having caregivers and appreciate those relationships. Some people reach the point that they don't really want to live and we do have a law in Vermont that allows a patient to hasten their death." Then listen for the level of information the patient might want about this.
- Be Clear that MAID is Totally the Patient's Decision: Be clear that a decision to consider MAID is never final. The patient can change their mind at any time.
- Hospice is a Great Complement to MAID: Encourage patients to consider hospice alongside MAID. Hospice providers have experience guiding patients through the decision and being with them through the date of ingestion.
Out of state clinicians
Physicians must be licensed in Vermont to have the legal protections of Act 39.
Many Vermont patients are served by doctors at Dartmouth Hitchcock Medical Center (DHMC) in New Hampshire. New Hampshire does not allow medical aid in dying.
However, DHMC Doctors who are Vermont Licensed Can Prescribe!
A DHMC doc with a Vermont license is allowed to assist an eligible Vermont patient with medical aid in dying if ALL activities related to Act 39 occur on the Vermont side of the border. This includes receiving the two oral requests from the patient and writing/calling in the prescription. It also means that a physician using telemedicine must do so while standing in Vermont. The actual location of the physician must then be documented in the patient record.
We recommend that doctors affiliated with DHMC who have legal or procedure questions contact the DHMC legal department.
Physicians Serving Non-Residents: If the patient is not a resident of Vermont, please see the guidelines on this page For Non-Residents.
Many Vermont patients are served by doctors at Dartmouth Hitchcock Medical Center (DHMC) in New Hampshire. New Hampshire does not allow medical aid in dying.
However, DHMC Doctors who are Vermont Licensed Can Prescribe!
A DHMC doc with a Vermont license is allowed to assist an eligible Vermont patient with medical aid in dying if ALL activities related to Act 39 occur on the Vermont side of the border. This includes receiving the two oral requests from the patient and writing/calling in the prescription. It also means that a physician using telemedicine must do so while standing in Vermont. The actual location of the physician must then be documented in the patient record.
We recommend that doctors affiliated with DHMC who have legal or procedure questions contact the DHMC legal department.
Physicians Serving Non-Residents: If the patient is not a resident of Vermont, please see the guidelines on this page For Non-Residents.
Clinicians employed by FQHCs or the VA
Federally Qualified Health Clinics and the Veterans Administration may have federally-imposed restrictions on what services their doctors can offer. Patients of these services who want to consider MAID should ask for a referral to a physician who can serve them.
What restrictions can institutions place on doctors or patients?
Act 39 prohibits health care facilities and health care providers from prohibiting doctors from participating in MAID. (Section 5285)
Act 39 does contain an "opt out" provision that states that a medical facility can have a published rule that prevents its own doctors from prescribing MAID where the intention is that the patient would ingest the medication in the facility. (Section 5286)
Therefore:
Act 39 does contain an "opt out" provision that states that a medical facility can have a published rule that prevents its own doctors from prescribing MAID where the intention is that the patient would ingest the medication in the facility. (Section 5286)
Therefore:
- Care Facilities: There is no legal basis for a residential care facility such as a nursing home or assisted living facility to have a policy prohibiting residents from using MAID, unless the prescription is written by a doctor who is an employee of the facility.
- Hospice: There is also no legal basis for a hospice organization to have a policy prohibiting its doctors from prescribing or consulting under Act 39.
- Hospice Residence: It is an open question whether a hospice residence could use the "opt out" provision of the law to have a policy against ingestion of MAID medications on the premises. If such an opt out policy is permitted, it would only apply if it were the Hospice Residence's employee doctor who was prescribing.
Additional Resources
Patient Choices Vermont (PCV) Helpline: To submit a Helpline request, please complete the form on our Contact Page.
Vermont Department of Health
American Clinicians Academy on Medical Aid in Dying (ACAMAID)
Vermont Medical Society Policy: On November 4, 2017, the Vermont Medical Society adopted a new policy statement on end-of-life care, recognizing Act 39 and medical aid in dying as legitimate options for patients, and respecting the individual choice of doctors to assist patients through the Act 39 process. The full resolution may be found here.
Vermont Department of Health
American Clinicians Academy on Medical Aid in Dying (ACAMAID)
Vermont Medical Society Policy: On November 4, 2017, the Vermont Medical Society adopted a new policy statement on end-of-life care, recognizing Act 39 and medical aid in dying as legitimate options for patients, and respecting the individual choice of doctors to assist patients through the Act 39 process. The full resolution may be found here.