Guidelines and Checklist for Non-Residents of Vermont and Their Doctors
|
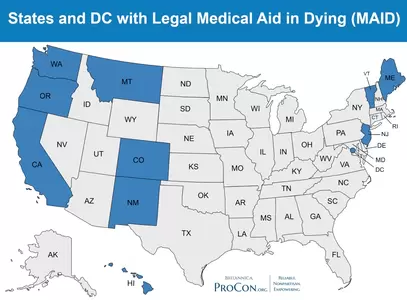
Vermont's Medical Aid in Dying Law (Act 39) is available to both residents of Vermont and non-residents. This page is specifically for non-residents.
Please be aware that the process is not quick or easy for people coming from out of state for medical aid in dying. There are many arrangements that must be made in a step-by-step process. If you are early in your terminal diagnosis, if you are relatively mobile, if you have the ability to do research and make the arrangements, then it is more likely that you will be able to access this care. Most people will find that having a group of supportive friends and family to assist them with tasks will be valuable. Please also be aware that there is no organization or person who will make all the arrangements for you. There is no "Program" as such.
We have carefully assembled the guidelines and checklist below and encourage you to study it carefully. Finding a Doctor: The most common request we receive is that we help a patient find a Vermont doctor. Please understand that PCV does not have a list and cannot refer you. You will have to make your own inquiries. Click here for a list of Medical Centers. |
|
The Vermont medical community is already working hard to serve its existing patients. Many areas of Vermont remain underserved with doctors and healthcare providers. Vermont's doctors may not be readily available to assist you with medical aid in dying. It may take some time to accomplish all that is required.
The Wayfinders Network:
PCV has established the Wayfinders Network, a collaborative group of retired hospice nurses, case managers, death doulas, and social workers who are available to help patients and their families.
Click here for more information and a list of Wayfinders who may be able to assist you.
PCV has established the Wayfinders Network, a collaborative group of retired hospice nurses, case managers, death doulas, and social workers who are available to help patients and their families.
Click here for more information and a list of Wayfinders who may be able to assist you.
|
Checklist for Patients |

2. Do You Meet All the Qualification Requirements
|
Evaluate whether you meet all the requirements of Vermont’s medical aid in dying law. You must:
Familiarize yourself with the requirements, including two oral requests, a written request and a second doctor's opinion. We suggest you download the PCV Guide to Medical Aid in Dying. |

4. Ask Your Doctor for Referral to a Vermont Doctor
|
You must establish a relationship with a Vermont-licensed doctor who is practicing in Vermont and who is able and willing to prescribe the end-of-life medication after you meet all of the requirements. Your Vermont doctor will need to assess your situation, make the appropriate findings and prescribe. Your prescribing doctor will also need to have you see a second Vermont-licensed doctor for confirmation that you meet the qualification requirements.
Finding a Vermont Doctor: The best way to connect with a Vermont doctor is by referral from your existing physician. Ask your doctor to approach your request like any other medical referral. If your doctor doesn't have specific contacts in Vermont, they should contact their equivalent department (oncology, neurology, etc.) at a medical facility in Vermont. If any doctors on your team need additional guidance, they can contact PCV for further guidance. Be aware that Vermont doctors will not be able to tell you over the phone if you will qualify. You must be willing to take the risk, and physically come to Vermont for medical consultations. Then, you will learn whether medical aid in dying will be available for you. Physicians employed by federally funded facilities such as the VA and FQHCs are not allowed to prescribe the medication. Also note that physicians have no legal obligation to participate in medical aid in dying. Patient Choices Vermont does not maintain a list of doctors to whom we can refer you. We can coach you on how to have a conversation with your doctor to request a direct referral. This is a list of medical centers that have doctors that may be able to assist you. A Vermont doctor will at a minimum require the following information in order to evaluate your case:
|
|
Guidelines for Doctors |
Caring for a patient who is considering medical aid in dying and their other end-of-life choices is the same regardless of whether the patient is a Vermont resident or from out of state. All patients must meet the Act 39 eligibility criteria and complete the required process. Please see the Clinician's Guide to Medical Aid in Dying.
All Steps Must be Taken Physically in Vermont. The patient will have to be physically present in Vermont for all parts of the process, including doctor meetings, formal requests and the receipt and use of the medication. TO BE CLEAR: Patients will not be able to have appointments by telemedicine from their home state and will not be able to take the medication to their home state. Doctors can determine whether telemedicine is appropriate for any of the consultations as long as they can confirm and record that the patient is physically in Vermont.
Why to Insist on Vermont Presence: Laws in other states may subject a patient, their family and friends to serious legal risks, especially if they take lethal medication home. In addition, Vermont-licensed doctors must stay within the scope of their licensure by serving patients who are physically present in Vermont. This may be difficult to confirm with telemedicine. Therefore, even though Act 39 does not specify that physical presence in Vermont is required, telemedicine must be used very cautiously.
Confirm and Re-confirm: It is recommended that doctors confirm and re-confirm at each visit that the patient has made suitable plans for the day of self-administration in Vermont. Please see the Checklist for Patients above.
Receiving Referrals and Requests: Patient Choices Vermont will be advising out-of-state patients to review their options with their existing medical teams, including a review of the Act 39 eligibility requirements. Our hope is that patients pursuing aid in dying in Vermont will be well-versed in the requirements and that their medical records will cover the information their Vermont doctors will need to provide this care.
If You Receive a Referral: You are always at liberty to accept or decline a new patient. If you do take a patient from out of state based on a referral, you can encourage the referring doctor to have the discussions outlined above in the Checklist for Patients. If they need further guidance, direct them to the Clinician's Guide to Medical Aid in Dying.
If You Receive a Call from a Patient: If an out-of-state patient calls your office seeking a doctor who can provide medical aid in dying, your staff can first suggest that they read the Checklist for Patients above. Your staff can also reiterate the importance of all steps being taken in Vermont. If the patient is clear that they meet the requirements and can handle the logistics, then you can decide whether to accept the new patient.
If You Would Like Training for Your Staff: Please contact PCV if you would like to arrange a video call for your staff to learn how to handle requests from patients or doctors' offices.
All Steps Must be Taken Physically in Vermont. The patient will have to be physically present in Vermont for all parts of the process, including doctor meetings, formal requests and the receipt and use of the medication. TO BE CLEAR: Patients will not be able to have appointments by telemedicine from their home state and will not be able to take the medication to their home state. Doctors can determine whether telemedicine is appropriate for any of the consultations as long as they can confirm and record that the patient is physically in Vermont.
Why to Insist on Vermont Presence: Laws in other states may subject a patient, their family and friends to serious legal risks, especially if they take lethal medication home. In addition, Vermont-licensed doctors must stay within the scope of their licensure by serving patients who are physically present in Vermont. This may be difficult to confirm with telemedicine. Therefore, even though Act 39 does not specify that physical presence in Vermont is required, telemedicine must be used very cautiously.
Confirm and Re-confirm: It is recommended that doctors confirm and re-confirm at each visit that the patient has made suitable plans for the day of self-administration in Vermont. Please see the Checklist for Patients above.
Receiving Referrals and Requests: Patient Choices Vermont will be advising out-of-state patients to review their options with their existing medical teams, including a review of the Act 39 eligibility requirements. Our hope is that patients pursuing aid in dying in Vermont will be well-versed in the requirements and that their medical records will cover the information their Vermont doctors will need to provide this care.
If You Receive a Referral: You are always at liberty to accept or decline a new patient. If you do take a patient from out of state based on a referral, you can encourage the referring doctor to have the discussions outlined above in the Checklist for Patients. If they need further guidance, direct them to the Clinician's Guide to Medical Aid in Dying.
If You Receive a Call from a Patient: If an out-of-state patient calls your office seeking a doctor who can provide medical aid in dying, your staff can first suggest that they read the Checklist for Patients above. Your staff can also reiterate the importance of all steps being taken in Vermont. If the patient is clear that they meet the requirements and can handle the logistics, then you can decide whether to accept the new patient.
If You Would Like Training for Your Staff: Please contact PCV if you would like to arrange a video call for your staff to learn how to handle requests from patients or doctors' offices.
|
FAQs: |
Q: Why must all steps be taken in Vermont?
A: Laws in other states may subject a patient, their family and friends to serious legal risks, especially if they take lethal medication home. In addition, Vermont-licensed doctors must stay within the scope of their licensure by serving patients who are physically present in Vermont. This may be difficult to confirm with telemedicine. Therefore, even though Act 39 does not specify that physical presence in Vermont is required, telemedicine must be used very carefully.
Q: Is the patient or family at legal risk in the patient's home state?
A: Legal risks for families and friends are minimized if all actions, including self-administration of aid in dying medication take place physically in Vermont, where legal protection is provided. Each state has its own laws. Individuals who are concerned about the laws of their own states should check with an attorney in their state.
Q: Will health insurance cover the cost of medical aid in dying?
A: In general, the cost of doctor visits for end-of-life consultations are covered by insurance. Some insurance covers the cost of medication; other policies and plans do not. You should check with your insurance carrier to evaluate what costs you may have to cover out-of-pocket.
Q: How does medical aid in dying affect my life insurance:
A: Per Vermont law, the cause of death reported on the death certificate of an individual using medical aid in dying is the terminal illness which qualified the individual to use it. We are not aware of any negative consequences for life insurance. For out-of-state residents, we suggest that you check with your insurance carrier.
A: Laws in other states may subject a patient, their family and friends to serious legal risks, especially if they take lethal medication home. In addition, Vermont-licensed doctors must stay within the scope of their licensure by serving patients who are physically present in Vermont. This may be difficult to confirm with telemedicine. Therefore, even though Act 39 does not specify that physical presence in Vermont is required, telemedicine must be used very carefully.
Q: Is the patient or family at legal risk in the patient's home state?
A: Legal risks for families and friends are minimized if all actions, including self-administration of aid in dying medication take place physically in Vermont, where legal protection is provided. Each state has its own laws. Individuals who are concerned about the laws of their own states should check with an attorney in their state.
Q: Will health insurance cover the cost of medical aid in dying?
A: In general, the cost of doctor visits for end-of-life consultations are covered by insurance. Some insurance covers the cost of medication; other policies and plans do not. You should check with your insurance carrier to evaluate what costs you may have to cover out-of-pocket.
Q: How does medical aid in dying affect my life insurance:
A: Per Vermont law, the cause of death reported on the death certificate of an individual using medical aid in dying is the terminal illness which qualified the individual to use it. We are not aware of any negative consequences for life insurance. For out-of-state residents, we suggest that you check with your insurance carrier.
If you need further clarification on any of this information,
you make contact PCV by submitting an inquiry form on our Contact Page.
PCV is an independent 501(c)(3) organization, not supported by any government agency.
While our services are free, our small staff and dedicated team of volunteers counts on individual donations to cover our month-to-month operations. Please, consider supporting the PCV team by making a donation.
Thank you.
While our services are free, our small staff and dedicated team of volunteers counts on individual donations to cover our month-to-month operations. Please, consider supporting the PCV team by making a donation.
Thank you.
This webpage is supported by individual donors and in part by Compassion and Choices.