|
On behalf of Patient Choices Vermont, we urge you to favorably consider S.1331/H.2246, An
Act Relative to End-of-Life Options. We are pleased to announce that on July 14, 2023, Oregon Governor Tina Kotek signed House Bill 2279, removing the residency restriction from Oregon’s Death with Dignity Act.
PCV co-sponsors Act 39 How would you react when your dearest friend who is dying of cancer, decides to hasten death and asks you to be present at the end of their life? 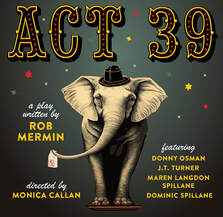 Act 39 Haybarn Theater, Goddard College, Plainfield, VT June 22 - July 2, 2023 A stage play by: Rob Mermin Directed by: Monica Callan Produced by and starring: Donny Osman Associate Producer and co-star: J.T. Turner with Maren Langdon Spillane and Dominic Spillane Music by: Johnnie Day Durand Please help us stay ahead of the curve. Donate today.On May 2nd, as a result of PCV's research, education and advocacy, the State of Vermont removed the residency requirement from our medical aid in dying law.
This landmark change is a huge step forward for compassion and end-of-life choice. Now, any patient who meets the requirements listed in Act 39 can come to Vermont to apply for this important option. In a huge step for compassion at the end of life, the State of Vermont has just opened the option of medical aid in dying to people regardless of where they live.
Removal of the Act 39 residency restriction is far more than a political victory. The overwhelming support in the legislature and signature by the Governor demonstrate how, together, we have accomplished a pivotal shift in cultural attitudes toward end-of-life choice here in Vermont. Since the founding of PCV twenty-one years ago, medical aid in dying has become a widely valued and respected option in the continuum of end-of-life care. Vermont’s Action Will Help Terminally Ill Adults in Other States Access Peaceful Dying Option Advocates for improving end-of-life care options for terminally ill adults praised the Vermont legislature and Governor Phil Scott (R-Vt.) for becoming the first state to remove the residency requirement from its medical aid-in-dying law.
Vermont is just one final step away from eliminating the residency requirement from our medical-aid-in-dying law, Act 39.  We extend our heartfelt thanks to members of the Vermont Senate who overwhelmingly passed H.190 yesterday. In particular, our thanks go out to Senator Ginny Lyons, Chair of the Senate Health and Welfare Committee, and the committee members who carefully considered this bill. We are pleased to report that the Vermont Senate Committee on Health and Welfare voted on Thursday, April 14, 2023 to recommend House Bill 190, which would remove the residency requirement from our medical-aid-in-dying law, Act 39. The bill now goes to the full Senate for a vote.
 Patient Choices Vermont (PCV) is pleased to celebrate the settlement of a lawsuit filed last August challenging the constitutionality of the Vermont residency requirement in our medical-aid-in-dying law (Act 39). The settlement means that plaintiff Lynda Shannon Bluestein, a terminally ill cancer patient from Connecticut, will now have access to medical-aid-in-dying services in Vermont. The settlement further stipulates that Vermont officials will support removal of the residency requirement from the law. Act 39, adopted in May 2013, enables terminally ill Vermonters who are capable of making their own medical decisions, to request and receive medication to bring about a hastened death at a time of their choosing. Act 39, like similar medical-aid-in-dying laws in other states, currently makes end-of-life choice only available to Vermont state residents. Josh Crane, reporter and producer for Brave Little State with Vermont Public says, "If you’re like me, you may not have realized Vermont is one of just 10 states with a Medical- Aid-in-Dying (MAiD) law on the books. Act 39, as it’s known here, passed in 2013. And there’s a bunch of criteria you must meet in order to use it, like being a Vermont resident over the age of 18 with a terminal illness."
|
Categories
All
Archives
July 2024
|
Proudly powered by Weebly


 RSS Feed
RSS Feed